What are the organs most affected by COVID‐19?
Coronavirus Infection: How Does It Affect Your Body?
A virus enters your body through healthy cells and infects them. The invader spreads throughout your body by making copies of itself. The virus predominantly enters the human body through the angiotensin-converting enzyme-2 (ACE2) and transmembrane serine protease 2 (TMPRSS2) receptors and nasal cavity cells of the respiratory system’s NT and then gradually moves towards the lung to initiate infection.
Given the undeniable association between viral and bacterial strain co-infections and respiratory disease stringency, there is an urgent need to understand better how relations of SARS-CoV-2 with the host microbiome in the respiratory tracts associate with viral infections that enable co-infection. The coronavirus attaches itself to receptors on healthy cells, particularly those in your lungs, with its spike proteins. Once inside, the coronavirus seizes control of healthy cells while some of the healthy cells are eventually killed.
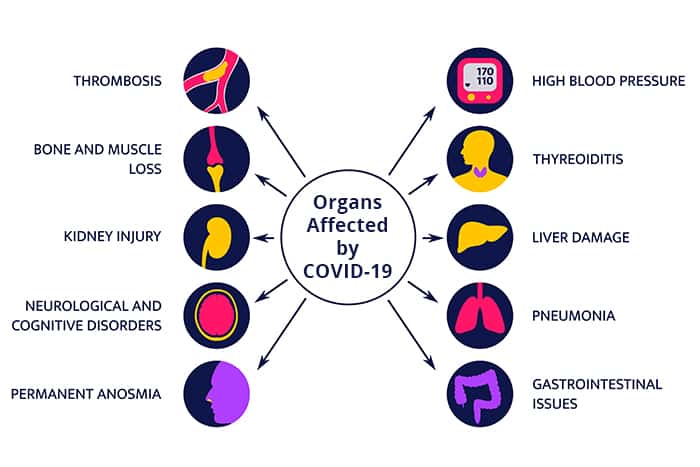
Organ damage caused by COVID-19
Even though COVID-19 is a disease that predominantly affects the lungs, it can also harm other body organs, such as the kidneys, brain and heart. Organ damage may result in long-term health problems post-COVID. Long-term breathing problems, heart complications, chronic kidney damage, stroke, and Guillain-Barre syndrome – a condition that causes temporary paralysis — are all possible long-term health impacts in some people.
Post COVID-19, some adults and children develop the multisystem inflammatory syndrome. Some organs and tissues become significantly inflamed in this situation.
Covid-19 Variants
The many thousands of SARS-CoV-2 variants are grouped into either clades or lineages. At present, the specialist group convened by WHO has suggested the labelling of variants using Greek Alphabets, for instance, Alpha, Beta, Delta, and Gamma, as it will be more accessible and more practical to discuss by non-scientific audiences. As of December 2021, there are five dominant variants of SARS-CoV-2 spreading among global populations:
- The Alpha variant (B.1.1.7), also known as the UK variant
- The Beta variant (B.1.351), also known as the South Africa variant
- The Gamma variant (P.1), also known as the Brazilian variant
- The Delta variant (B.1.617.2), also known as the Indian variant
- The Omicron variant (B.1.1.529)
In November 2021, the world health organisation (WHO) designated variant B.1.1.529, Omicron’s variant of concern. Omicron has several mutations that may impact how it behaves, for example, how easily it unfurls or the severity of illness it causes. However, individuals infected with the omicron variant indicate that the new covid-19 variant does not target lung tissue as aggressively as others.
Human coronaviruses were first characterized in the 1960s and are responsible for a substantial proportion of upper respiratory tract infections in children. SARS-CoV, human coronavirus NL63 (HCoV-NL63) and HCoV-HKU1 were first described in 2003, 2004 and 2005, respectively. The Discovery of three new human coronaviruses does not represent a sudden increase in emerging infections by new coronaviruses. Only SARS-CoV has recently been introduced to the human population; the other two have been circulating in humans for a long time.
Before the COVID‑19 pandemic, an established body of knowledge existed about coronaviruses’ structure and function, causing diseases like severe acute respiratory syndrome (SARS). This knowledge accelerated the development of various covid-19 vaccination platforms. Several testing methods have been developed to diagnose the disease.
The standard diagnostic procedure is by detection of the virus’s nucleic acid by real-time reverse transcription-polymerase chain reaction (rRT-PCR), transcription-mediated amplification (TMA), PCR test, or by reverse transcription loop-mediated isothermal amplification (RT-LAMP) through nasopharyngeal swab.
The organs most impacted by COVID-19, both at the moment of infection and in terms of long-term effects, are listed below.
1. Heart
Some of the other familiar COVID-19 symptoms include:
- Palpitations,
- Fatigue and
- Chest pain
This is because COVID-19 also impacts the heart, and a lasting impact on the heart of the COVID-19 patient is widespread. The grouping of blood clots in the heart also poses risks of heart attacks or strokes. It can also cause problematic blockages in the heart in the long run. Therefore, patients of COVID-19 should consult a heart specialist, especially if they have any associated problems like cholesterol, diabetes, etc.
2. Liver
COVID-19 frequently affects the liver of those who are infected with it. After individuals have recovered from COVID-19, there have been reports of increasing enzyme levels. It can potentially cause liver dysfunction. The most visible and widespread ailment resulting from this is digestive troubles.
Not only can the coronavirus harm the liver, but so can the high doses of medication given to the patient throughout their treatment. This is why, if there are any underlying conditions, it is also a good idea to be cautious with medications and visit a doctor.
3. Lungs
COVID-19 is primarily a respiratory disease; therefore, it’s no surprise that it affects the lungs. Two of COVID-19’s most common symptoms are shortness of breath and chest pain. These are symptoms that COVID-19 people have even after the initial infection has subsided.
This is due to the coronavirus’s damage to the lungs and other tissues, which puts respiratory health at risk. This cause is why it’s crucial to get sufficient rest while you’re sick with COVID-19 and after that so that your respiratory system can repair adequately.
4. Brain
COVID-19, contrary to popular perception, can also influence the patient’s brain. This applies to mental health issues, which are formidable in and of themselves, and to other problems such as inflammation. This can lead to seizures in most threatening situations and other common and seemingly minor issues, including cognitive fog, dizziness, persistent headaches, and more. COVID-19 has a long-term effect of constant weariness, which can substantially impede everyday life functions.
What Else Does COVID-19 Do to Your Body?
Some people also have symptoms including:
- Pinkeye
- Rashes
- Liver problems or damage
- Heart problems
- Kidney damage
- Dangerous blood clots, including in their legs, lungs, and arteries.
- Some clumps may cause a stroke.
Table 1: List of body parts affected by COVID-19 and its harmful effects
| Body organs/parts | Damage/Consequences | Acts on/ Type of cell affected |
| Gut dysbiosis | Decrease probiotic microorganisms | Inflammation and diarrhoea | The small intestine, enterocytes, colon |
| Acute Kidney Injury (AKI) | Podocytes and proximally straight tubular cells | |
| Rhabdomyolysis,hypoxemia,and coagulopathy | Glomerular cells, tubular epithelium, and podocytes | |
| Irregular liver function | Cells of the bile duct | |
| Microvascular disorders | Pericytes | |
| Myocarditis | Myocardium | |
| Acute Coronary Syndrome | Endothelial cells | |
| Alveolar damage, hypoxemia | Alveolar cell | |
| Acute Respiratory Distress Syndrome | Hyper fusion of alveolar cells | |
| Cerebral haemorrhage | ACE-2 receptor affected due to amplified blood pressure | |
| Encephalitis | Neuronal destruction and nerve tissue lesions | |
| Puzzlement, loss of awareness, coma | Cerebral capillary endothelial cells |
Immune Response
According to researchers, the virus could connect a weak immune response beyond the respiratory tract to less efficient virus clearance in organs outside the pulmonary system. Some researchers have claimed that patients who died more than a month after symptom onset had SARS-CoV-2 RNA in their brains.
Focusing on different parts of the brain can help understand neurocognitive impairment, also known as “brain fog,” and other neuropsychiatric manifestations of long-term COVID. SARS-CoV-2 should be regarded as a systemic virus that can be clear in some persons but can remain for weeks or months in others, resulting in protracted COVID, a complicated systemic disease.
Conclusion
ACE-2 has several activities in COVID-19 pathophysiology that directly impact illness therapy and outcome. Microbiota dysbiosis and weakened intestinal blood vessels are significantly associated with the development of atherosclerosis and an increased risk of death in individuals with CVDs, obesity, diabetes, or chronic renal illnesses. Furthermore, Acute Kidney Injury (AKI) may cause gut dysbiosis in COVID-19 patients.
As a result, COVID-19 patients should get a neurological checkup as soon as possible, especially if they have symptoms such as cerebrovascular infections, consciousness, or paresthesia. However, there is no specific treatment for coronavirus SARS CoV-2 infections. As a result, primary intensive care is required to recognise vital indications, maintain blood pressure and oxygen levels, and treat and manage various consequences such as secondary infections and organ failure.
Visit the Helvetica Health Care website to learn more about bacterial strains that expand our collection of viruses and bacteria. Our new products are available in various formats to meet research and product development needs.
